How Our SOAP Notes Template Works
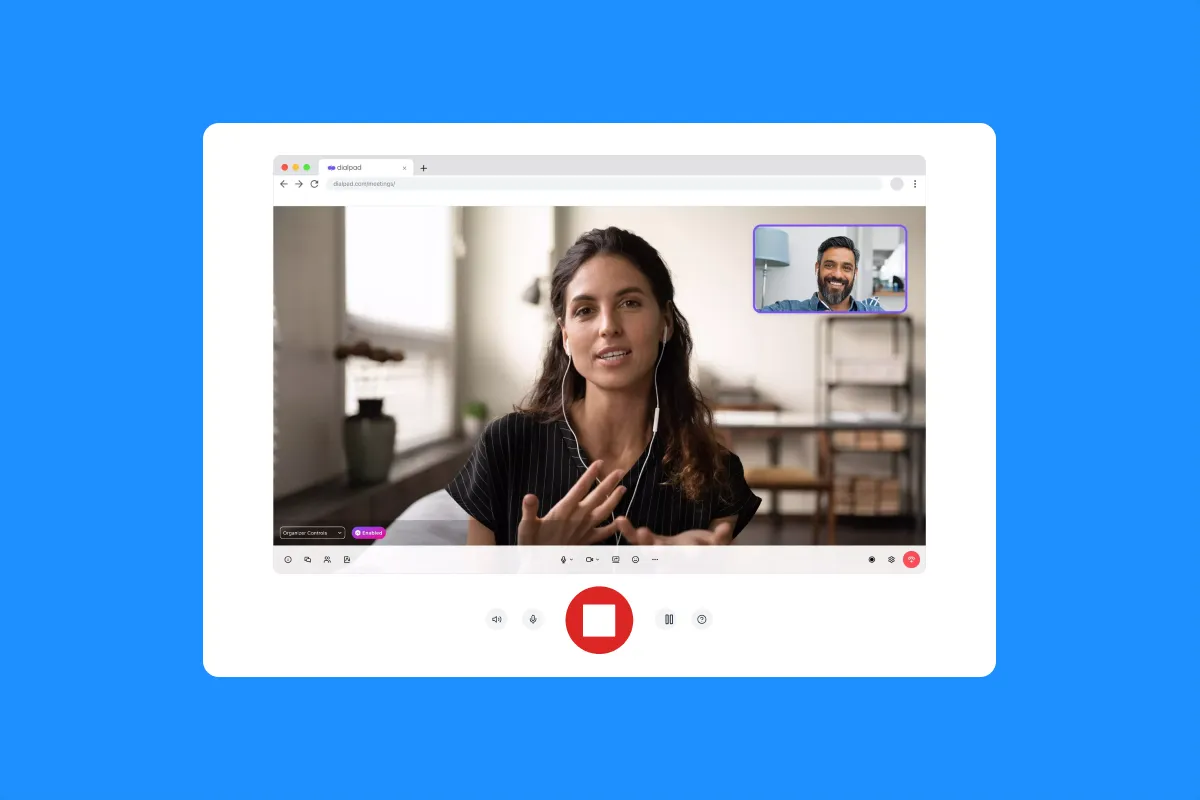
- Record the Patient Session: Securely capture the audio from your telehealth or in-person patient encounter.
- Get a HIPAA-Compliant Transcript: Receive a fast, accurate, and secure transcript of the conversation.
- Generate the SOAP Note: Our AI, trained on medical terminology, analyzes the transcript and organizes the information into the four sections of a SOAP note: Subjective, Objective, Assessment, and Plan.
- Review and Finalize: Quickly review the AI-generated note for accuracy, make any necessary edits, and sign off.
- Export to EHR: Export the completed note and upload it directly to your Electronic Health Record (EHR) system.
This process transforms your patient conversations into compliant, structured documentation with minimal manual effort.
Benefits of a SOAP Notes Template
Writing SOAP notes is essential for quality patient care, but it’s also one of the most time-consuming tasks for healthcare professionals. The biggest challenge, especially after a telehealth appointment, is documenting the session accurately and efficiently. Our AI-powered SOAP notes template solves this problem by automatically generating a structured note from your session recording.
This allows you to focus on the patient during the encounter, not on taking notes. It drastically reduces documentation time, ensures accuracy, and provides a consistent format for every patient record.
Who Needs a SOAP Notes Template?
This tool is designed for any clinician or healthcare provider who needs to document patient encounters:
- Doctors and Physicians who want to reduce their administrative burden and spend more time with patients.
- Nurses and Nurse Practitioners who need to efficiently document patient visits and updates.
- Therapists and Mental Health Professionals who need to capture detailed subjective information from their sessions.
- Medical Scribes looking to improve the speed and accuracy of their documentation.
FAQ
Is this SOAP note generator free?
Our basic template for transcribing and structuring your patient encounters into a SOAP note format is free to use for a limited number of sessions.
Is this tool HIPAA-compliant?
Yes. We take patient privacy and security very seriously. Our systems are designed to be HIPAA-compliant, ensuring that all patient health information is handled securely.
How does the AI understand medical terminology?
Our AI has been specifically trained on a large corpus of medical conversations and terminology, allowing it to accurately identify and categorize the information from your patient sessions into the correct SOAP format.
Can I customize the template for my specialty?
The SOAP note format is standardized (Subjective, Objective, Assessment, Plan). Our tool automatically organizes the conversation into these four sections. You can then easily edit the content within each section to fit the specific needs of your specialty.
Does this integrate directly with my EHR?
Our tool allows you to export the completed SOAP note in a standard format that can be easily uploaded or copied and pasted into any major EHR system, ensuring a seamless fit into your existing workflow.